Helping Cancer Researchers Jump the Last Hurdles Before Clinical Trials
Developing a new cancer drug takes years of hard work and substantial financial support. That’s why some innovative ideas don’t make it through the final stretch to their ultimate destination—new drugs in the hands of cancer patients.
“It can be especially hard for scientists to get funding for research that’s close but not quite ready for clinical trials,” said Susanna Greer, PhD, a Scientific Director at the American Cancer Society (ACS). Those trials are the final requirement before a new drug or other treatment is submitted for FDA approval so it can be prescribed to patients.
The ACS Mission Boost Grant takes aim at that hurdle. These grants go to researchers who either have current ACS grants or have gotten them in the past. “The Mission Boost grant helps rescue science that sometimes falls into the valley of death, where promising research comes to an abrupt end because it otherwise can’t get the funding it needs to cross the bridge between discovery and helping patients,” said Greer.
Giving Chemo Side Effects the Red Light
Mei Wu, MD, PhD, is one of the new recipients of a Mission Boost grant. As a doctor and cancer researcher, Wu understands the toll that cancer treatment can take on the body. Loss of appetite, nausea, vomiting, diarrhea, and weight loss are common side effects of certain types of chemotherapy. If severe enough, these problems can delay treatment for some patients, too.
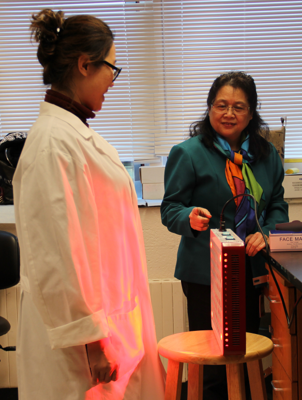
Dr. Wu (wearing scarf) chats with her research fellow as she demonstrates light therapy from the low-level laser they’re testing to ease intestinal side effects from some types of chemotherapy.
“Chemotherapy weakens the whole body,” said Wu, who is a researcher at the Wellman Center for Photomedicine in Boston. “Some patients may have to regain their strength and some weight before they can start another chemotherapy cycle.”
It hit Wu hard when her friend was being treated for pancreatic cancer and suffered through these side effects. “Each time I took him and picked him up from the hospital, I saw the stress his body was under. He was weak, and he lost lots of weight,” she said.
Wu hopes that low-level laser light therapy will be able to eliminate or greatly reduce treatment-related side effects. The infrared light boosts activity in the part of the cell that makes its energy, called mitochondria.
If light therapy improves patients’ recovery between chemotherapy cycles, it will be very significant because it’s drug-free, and it’s cheap.”
Previous research has suggested that laser light therapy can stimulate hair growth and may speed the healing of burns in skin cells. Wu hopes it can bring the same benefits to cells in the gastrointestinal (GI) tract that have been damaged by chemotherapy and help patients heal faster between their treatments.
“When patients already have a lot of chemo drugs in their body, giving them more drugs to treat GI issues could cause other side effects for them,” Wu said. “If light therapy improves patients’ recovery between chemotherapy cycles, it will be very significant because it’s drug-free, and it’s cheap.”
Now, the doctor-scientist is working with engineers to create a device that they can test in clinical trials. The plan is to test it in patients who will give themselves light therapy at home, for about an hour a day, throughout the course of their chemotherapy.
If it works, Wu hopes the therapy can help improve the patients’ quality of life, cut down on treatment interruptions, and help them get better results from their cancer treatment.
Disarming Resistant Cancer Cells
Randy Kimple, MD, PhD, believes that one drug meant to treat head and neck cancer may sometimes help the cancer cells survive instead.
Cetuximab (brand name Erbitux), a common targeted therapy drug that some patients with head and neck cancer receive, kills cancer by attaching to a specific substance in certain types of cancer cells. But it can also trigger a recycling process in cells called autophagy.

Randy Kimple, MD, PhD, holds cell survival assays that show cancer cells (the control) compared with cancer cells treated with cetuximab, with an autophagy inhibitor, and with a combination of the two.
In healthy cells, autophagy is a normal and needed process that allows the body to rid itself of damaged cells and make new ones. Autophagy is triggered when the body is experiencing stress, such as when a person’s taking a drug to treat cancer.
Some cancers take advantage of autophagy to give the tumor cells time to heal after the damaging effects of anti-cancer drugs. That healing time allows some cancer cells to survive treatment instead of dying as expected. Kimple and his colleagues have seen this in cells in petri dishes as well as in animals.
Collecting and studying patient biopsies is a crucial step towards identifying new drugs to treat cancer. But it's a step that's hard to fund."
Kimple and his research team are trying to learn whether drugs that block this recycling process could improve head-and-neck patients’ chances of survival.
As part of a clinical trial at University of Wisconsin, where Kimple is an associate professor of human oncology, doctors will biopsy patients’ tumors to confirm a diagnosis. Then the patients participating in the clinical trial will take cetuximab therapy. After 2 weeks of this treatment, the doctor will take a second biopsy.
Researchers will compare the biopsies to see if the treatment killed cancer cells or if it didn’t. They’ll also look at whether the level of autophagy in the biopsies taken after treatment is higher in patients whose tumors didn’t respond to the drug. If it is, then that might mean that increased autophagy is a sign that this particular treatment is not killing cancer cells as it should. That, in turn, could suggest that another drug to stop cetuximab from causing autophagy could help it work better.
Collecting and studying patient biopsies is a crucial step towards identifying new drugs to treat cancer. But it’s a step that’s hard to fund, Kimple said.
“When a drug company decides that they want to invest in autophagy-inhibitors, or whatever the drug may be, then there’s money available,” said Kimple. “But when the research is at this phase, when you’re first trying to prove that autophagy is a good target to go after, that part is harder to get funded.”
The results of the biopsy studies, along with additional mouse studies, might make the case for a clinical trial in humans to test how people with head and neck cancer respond to a combination of current treatment and autophagy inhibitors. Kimple hopes the drug combo could one day change the outlook for the more than 65,000 people who develop a type of head or neck cancer each year.
Maybe One Size Should Fit All in Pancreatic Cancer Treatment
Jordan Winter, MD, is a lone wolf in his approach to cancer treatment. “It seems like everyone is focused on targeting a subset of cancers with precision medicine,” he said. “I want to develop a drug that works against all pancreatic cells, not just some.” He believes he’s found a target for such a drug.
Precision medicine in cancer care is a personalized approach to treating cancer based not only on its type and stage, but also on the genetic makeup of the tumor. For example, in certain tumors, tests might show a change in a specific gene. In some cases, a treatment can target, attack, and kill only the cancer cells that have that specific gene.
Winter thinks one drug might work against all cancers in the pancreas, though, because all the cancer cells are deprived of nutrients. Typically, a tumor’s survival depends on the cells and other substances that live around it, in what’s called its microenvironment. Tumors in the pancreas, however, live in a barren microenvironment that has limited nutrients. In fact, conditions in this biological desert lead to the production of toxic waste that could kill the cancer cells. Except the toxic waste doesn’t seem to affect them.

Jordan Winter, MD, and a research colleague use the Seahorse XF analyzer to study the impact of the IDH1 inhibitor on mitochondrial function.
This is the most exciting discovery that I’ve been a part of in my career. To think that we’re only about 18 months away from a clinical trial – it can’t get here soon enough.”
Pancreatic cancer cells with higher levels of the normal IDH1 gene (which gives the body instructions for making the IDH1 enzyme) can thrive in the environment’s toxic waste–sometimes even in the face of a chemotherapy attack.
In research funded by a previous ACS grant, Winter discovered how cancer cells survive these conditions in the pancreas. They take advantage of an enzyme, called IDH1, which neutralizes the toxins, acting like a bodyguard for the cancer cells.
When Winter deleted the IDH1 gene from pancreatic cancer cells (using CRISPR), they essentially lost their bodyguard and could no longer defend themselves against standard chemotherapy drugs, allowing chemo to work and kill the cancer cells.
Now, with the help of the ACS, Winter and his team are testing an existing drug that blocks the normal IDH1 gene. Without that gene and its enzyme bodyguard, the cancer shouldn't be able to adapt to survive in its harsh environment with little oxygen and nutrients. So the cancer cells are expected to die in the toxic waste in the pancreas.
Winter said the drug is less toxic than chemotherapy and has few sides effects in mice. The drug works best under conditions with low nutrients, like the tumor microenvironment.
“In mice, the blocker works well alone, but we don’t know yet if patients will also need chemotherapy,” he said. “Even though that will increase the treatments’ toxicity, we think they will be great as a combo.”
Over the next 18 months, the Mission Boost grant will help fund the remaining tests that Winter must complete in mice. If all goes well, a Secondary Mission Boost grant will help support the human clinical trial. And if the results are positive in clinical trials for pancreatic cancer, Winter thinks the drug might work in breast and colon cancer too, since they also have an oxygen- and nutrient-deprived microenvironment.
“This is the most exciting discovery that I’ve been a part of in my career,” said Winter, who is a pancreatic cancer surgeon at University Hospitals in Cleveland, Ohio. “To think that we’re only about 18 months away from a clinical trial – it can’t get here soon enough.”
Driving Out “Hidden” Breast Cancer Cells
Cancer is most likely to come back within the first 5 years after treatment ends, so most people who have been cancer-free for that long are considered cured. “But for people with breast cancer,” said Dorothy Sipkins, MD, PhD, “there’s no time when they’re completely free from the chance of recurrence. Even if she realizes that, a woman is devastated if she’s been free of breast cancer for 10 years, then relapses.”
Sipkins and her research team at the Duke University School of Medicine in Durham, North Carolina, previously discovered how breast cancer cells are able to find a hiding place in the bone and eventually cause a relapse.

Dorothy Sipkins (in red), her lab team, and their mascot, Eleanor, hiking in Hillsborough, North Carolina.
Cancer is most likely to come back within the first 5 years after treatment ends, so most people who have been cancer-free for that long are considered cured. “But for people with breast cancer,” said Dorothy Sipkins, MD, PhD, “there’s no time when they’re completely free from the chance of recurrence. Even if a woman realizes that, she's devastated if she’s been free of breast cancer for 10 years, then relapses.”
Sipkins and her research team at the Duke University School of Medicine in Durham, North Carolina, previously discovered how breast cancer cells are able to find a hiding place in the bone and eventually cause a relapse.
Cancer cells can break away from the primary tumor in the breast and enter the bloodstream, travelling into a special tiny blood vessel inside the bone marrow called a sinusoid. The cancer cells latch onto a molecule called E-selectin on the sinusoid’s inner surface. Then, the breast cancer cells force their way through the blood vessel wall into the bone marrow.
Once they’re inside, Sipkins suspects that a molecule called SDF-1 helps protect breast cancer cells, allowing them to stay in the bone marrow. These tiny breast cancer cells, called micro-metastases, essentially hide out there for years before causing a cancer relapse. And anti-cancer drugs may be less likely to destroy them while they’re in the bone marrow.
Sipkins’ team has used two methods to stop this process from happening in mice. One was preventing breast cancer cells from getting into the bone marrow by using a drug (GMI-1359) to stop them from latching on to E-selectin.
Her team used the same drug to block the SDF-1 molecule, so it could no longer help the cancer cells stay in the bone marrow. That essentially forced cancer cells out of their hiding place and back to the bloodstream where chemotherapy drugs could better kill them.
Sipkins is using her Mission Boost Grant to learn whether this experimental medicine that blocks both E-selectin and SDF-1 can improve response to cancer treatment – be it chemotherapy, hormone therapy, or immunotherapy. If the drug brings good results in mice, her next step will be to test it in breast cancer patients.